Patients in need of urgent medical attention are still subject to a postcode lottery where the quality of care depends on where they live, MPs have warned.
There are still wide variations in ambulance response times depending on region, MPs on the Public Accounts Committee (PAC) said, as they found performances in key services had fallen “far below the standard the NHS says patients should expect and receive”.
It said that despite the NHS having “more money and staff than ever before”, it had made “poor use” of its resources to improve access for patients.
The committee said that although the NHS budget in 2023-23 came to £152bn – £28bn more than in 2016-17 – the performance of urgent and emergency care services “has been deteriorating for many years”.
Productivity, which had been improving before the COVID-19 pandemic, subsequently fell 23% over the two years from 2019-20 and 2020-21, the MPs noted.
Number 10 says drop in small boat crossings not due to weather – politics latest
The PAC report comes after the NHS waiting list in England hit a record high, with an estimated 7.75 million people waiting to start treatment at the end of August – up from 7.68 million in July.
The committee’s inquiry also examined delays in hospital discharges, which increased to an average of 13,623 patients in the fourth quarter of 2022-23 from 12,118 people during the same period the previous year.
Dame Meg Hillier MP, chair of the committee, said: “Anyone who has had recent contact with the NHS knows it is in crisis.
“Patients suffering long waits and hard-pressed staff working in a system which is not delivering deserve better. The PAC’s role is to analyse the underlying numbers, and attempt to provide a ‘get well soon’ plan for the NHS.
“The government and health system need to be alert to the serious doubts our report lays out around the workforce crisis, both the approach to tackling it now and the additional costs of funding it in the future.”
The PAC report found that people in some parts of the country are having to wait, on average, more than three minutes longer for an ambulance to arrive when they are facing a life-threatening emergency.
In 2021/22, average ambulance response times for the most serious incidents, including cardiac arrests, varied from six minutes 51 seconds for the London Ambulance Service to 10 minutes 20 seconds for the South Western Ambulance Service.
Ambulances aim to respond to the most serious life-threatening injuries and illnesses in an average time of seven minutes.
Along with variations in ambulance response times, the report also highlighted issues with sending patients home when they no longer need hospital care.
The length of stay in the worst-performing areas for discharging medically fit patients is more than double that of the best-performing areas, according to the report.
“Not enough [is] being done to address the systemic issues with discharges that lie within the gift of the NHS and its hospitals, and which cannot be blamed on external factors,” the MPs said.
“The NHS has not met targets for ambulance handovers since November 2017 and for A&E waits since July 2015, with wider declines in performance across the board.”
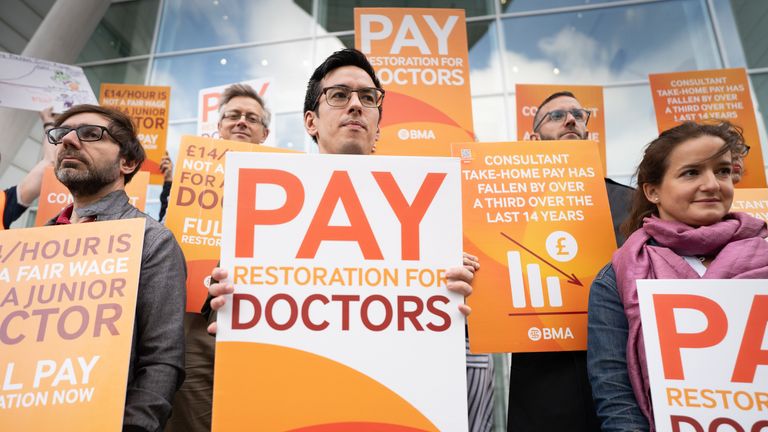
Meanwhile, they said the NHS’s long-term workforce plan includes only a commitment of an additional £2.4bn to cover training costs for the first five years of the 15-year plan.
The MPs said they were “unconvinced” by NHS England’s approach to address workforce shortfall, saying its desire to retain 130,000 staff who would otherwise leave over the next 15 years was an “aspiration which seems highly doubtful”.
Professor Julian Redhead, NHS England’s national clinical director for urgent and emergency care, said: “While this report includes data which is more than two years old and coincided with a once-in-a-generation pandemic, it is right to note the NHS has been under increasing pressure with staff experiencing record A&E attendances, hospitals fuller than at any point in their history and with thousands of beds taken up each day, in part, due to pressures in social care.
“It is testament to the hard work of staff and results of our NHS winter plan – rolling out 800 new ambulances, 10,000 virtual ward beds and work towards 5,000 extra core beds – that waiting times for ambulances, 999 calls and in A&E have improved across the country during this financial year.
Read more:
Expectant mothers and patients needing emergency treatment at risk of harm because of failing NHS care
Welsh government outlines cuts to protect NHS budget amid ‘unprecedented pressures’
“This progress has come as the NHS has committed to delivering £12 billion of annualised savings by 2024/25 – all while dealing with more than 100,000 staff posts being vacant.”
Royal College of Nursing Director for England, Patricia Marquis added: “Another day, and yet another report into failing NHS services that cannot keep patients safe.
“Nursing staff have been sounding the siren on staff shortages for years, but the government remains more focused on soundbites than solutions.
“We need the government to take urgent action, to stop our nursing staff leaving the profession. Patient care demands it. We are crying out for funding and detail on the workforce plan – there is still very limited progress on closing the gap in nursing vacancies.”
The Department of Health and Social Care has been approached for comment.