To get one thing clear at the start: I’ve never done a triathlon. I’ve never climbed a mountain or swum the Channel. I’ve never been on a hiking holiday.
Why am I telling you this? Because normally articles about long COVID start by describing the physical feats that sufferers are no longer able to perform.
Look, the writers say. Once, these people were so healthy they ran ultra-marathons in their spare time. Now they can barely make it to the shops.
It’s not wrong exactly, but to me it always struck a false note, because when long COVID is leeching my energy, it’s not the big things I miss, it’s everything else.
Energy to read or watch a show on TV. Energy to make plans and see them through, or be spontaneous. Energy to spend time peacefully with people you love. Energy to feel anything that isn’t crushing fatigue.
I recently met a teenager called Victoria, who came down with long COVID fifteen months ago, shortly before her twelfth birthday. In a tiny voice she said: “I didn’t get to be 12. I didn’t get to be 13 either. I just hope I get to be 14.”
What do you miss the most? I asked her. Victoria gave a miserable shrug. “Life,” she replied.
Long COVID is an incredibly diverse condition and in many ways my experience was very different to Victoria’s – yet with that one word she summed it up perfectly.
Eighteen months ago, I wasn’t running ultra-marathons, but I had a partner, a two-year-old son and a busy full-time job, and to be honest that was quite enough.
I never felt I had enough time and I would occasionally complain about being tired, but in retrospect I had energy to burn.
It wasn’t just that I could get up in the middle of the night to cuddle a crying child, then do live TV the next day – not well, but not so badly that too many people commented. I constantly performed astonishing physical and mental feats without even noticing.
I did more than one thing at once, often at high speed. I concentrated intensely, sometimes for hours on end. I was able to finish one job, then start immediately on another, even if it was just changing a nappy then taking the bins out.
I ambled through life secure in the knowledge that I was basically well, knowing that, if I was tired, sleep would restore me.
Then, in March 2021, two months before I was due to get my coronavirus vaccine, all that came to an end.
The change struck like a bolt of lightning from a clear blue sky. I’d been under the weather for a couple of weeks – nothing major, just a persistent cough, but for some reason I couldn’t seem to shift it. I took a day off work and carried on. Until 19 March, when I woke up and everything was different.
I was tired – overwhelmingly, crushingly tired, as if I’d been up for days, when in fact I’d slept all night – and I couldn’t think straight. When I tried to text my boss to tell him I wasn’t going to be able to make it into work, it took me more than an hour to string a sentence together.
Eventually, I got out a short apologetic message. Then I went back to bed, where I stayed for three days straight. It should have been scary, but I was too tired to be scared. The need for rest overwhelmed every thought or feeling.
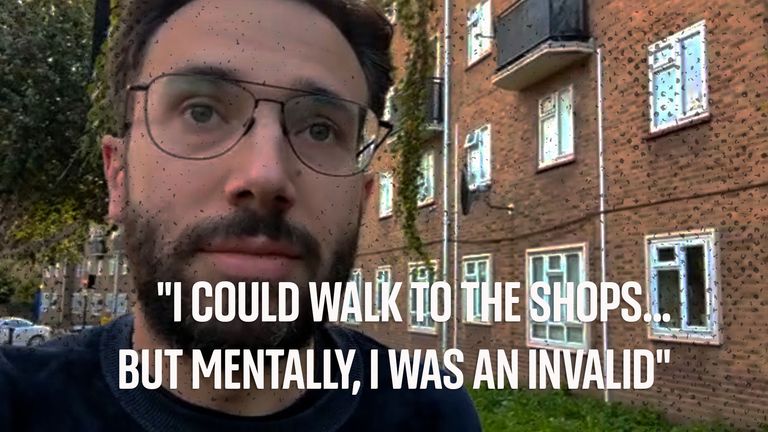
After a few days, I scraped myself out of bed, feeling a little fresher. “I’ll just check in on my emails,” I thought, anticipating my return to work, which surely couldn’t be far away now.
When I opened my inbox, tiredness hit. It really did hit, it was that strong and sudden. Words like fatigue didn’t begin to describe it. It was as if someone had reached inside me and turned me off at the mains.
Worse, it took me a week of bed rest just to get back to the point I’d been at before. It was a brutal introduction to the iron law that would rule my life from now on: if I pushed myself too hard, then I would pay for it.
Read more:
The debilitating after effects of coronavirus
Three types of long COVID identified with different symptoms
When I spoke to the GP a few weeks later, he wanted me to push myself. He suggested I start gradually increasing my levels of activity. He called this “graded exercise therapy”.
The consultation, held over the phone, was not reassuring. The doctor didn’t seem very interested in fatigue or brain fog. He quizzed me about my reaction to walking and running. “Are you sure you don’t have trouble breathing?” he asked, several times.
I didn’t. My problems were mainly cognitive, not physical. Once I got over the initial wave of exhaustion, I could walk to the shops and watch my son in the park. But mentally, I was an invalid.
I made my living writing and talking, but both of those activities were now as draining as running a marathon. A 15-minute phone conversation would wipe me out for the day. As soon as I tried to concentrate or focus, energy would drain out of me like air from a punctured tyre.
This explanation didn’t seem to impress the doctor. Without a concrete physical problem he told me he couldn’t refer me for immediate treatment.
“What about the long COVID clinics?” I asked. Just recently I’d read that the government had given the NHS funding for specialist treatment centres.
“You’ll need to have symptoms for three months,” the doctor said. “If you’re still experiencing problems then, call back and I’ll see what we can arrange.”
It seemed so far off I doubted it would be relevant, especially as I could work on building up my stamina. But when I tried to follow a graded exercise guide I found online – the GP just told me to do a bit more every day – it made me feel awful. Instead of building as I’d hoped, my strength was being sucked away.
Many long COVID sufferers had similar complaints. Graded exercise therapy was, I learned, incredibly controversial among sufferers of post-viral fatigue, ME, chronic fatigue syndrome and other similar disorders, who believed it made it harder to recover. There was even a name for the way exertion made my symptoms worse: post-exertional malaise.
Long COVID is an umbrella term that encompasses a dizzying range of symptoms and conditions, ranging across every human organ system, and it is still not clear whether it is one disease or a number of different diseases. Yet one common feature across almost all the symptom groups is this almost allergic reaction to over-exertion.
“I can’t emphasise sufficiently how important rest is,” says Danny Altmann, professor of immunology at Imperial College London,
“Increasingly we’re trying to get on with our lives, aren’t we, and ignore COVID and ignore COVID infections and reinfections. And part and parcel of that is, oh, just ignore it and, you know, power through it. I can only say, as somebody who spent the last two years thinking about long COVID, that that’s really the worst thing you could do.”
Abandoning graded exercise was relatively easy. The GP hadn’t given me a schedule, so I didn’t have anything to stick to, and after a while I simply gave up. Stopping other kinds of exertion was much harder. Perhaps if my problems had been physical, I might have found it easier to hold back, but I needed to stop myself thinking too hard. How do you go about doing that?
I tried repeatedly to start back to work, but every time I did I ended up in a state of collapse.
My bosses and colleagues could not have been more supportive and never put me under pressure to do more, but they were not equipped to stop me overdoing it, and I was not able to stop myself.
On one occasion, I rushed to meet a deadline, only to find myself so exhausted I was physically unable to read my son the ten-word sentences of The Tiger Who Came To Tea. Once again, I needed days in bed to recover.
None of this was constant. Long COVID is a disease that ebbs and flows, so I would have good days when everything seemed brighter, and every time I did I convinced myself I was on the mend. Strange as it may seem, I just didn’t realise how bad I really was. The reality only hit home nine months later when I’d finally recovered enough to speak to my partner about her experience.
On the outside, she told me, I seemed more or less like myself, if a little older and greyer. But when she tried to talk to me about anything more complex than the weather, my brain would start shutting down. “It was like you were drunk,” she said – not just because I was incoherent, but because I didn’t understand how incoherent I was.
Studies into the many symptoms of long COVID tend to group sufferers into three different categories: cardiovascular, respiratory and neurological. My brain problems left me unable to recognise my brain problems. I was so slow, I couldn’t see how slow I was.
This was a hard truth to discover. It pains me more than I can say to think about the burden I’ve placed on my partner, who has borne it with incredible patience and fortitude. She, and tens of millions of other hard-pressed carers, is as much a victim of long COVID as I am.
What energy I did have during this period, I put into chasing after treatments.
I went to an eye-wateringly expensive private clinic, where an exhaustive series of tests found that, medically speaking, I was in perfect health. I tried dozens of supplements suggested by people on social media, and spent an hour a week in a hyperbaric chamber, trying to increase the level of oxygen in my blood.
None of it made any obvious difference, unless you count an upset stomach, and after every failure I felt like a fool for pursuing treatments without any scientific backing. But what else was I meant to do? There was no evidence either to prove or disprove the effectiveness of these treatments, because they had never been studied in sufficient depth. Like every other long COVID sufferer, I was off the map of scientific knowledge, on my own, experimenting on myself.
Eventually, 15 months after my first symptoms, I managed to get an appointment at an NHS long COVID clinic, where I hoped to get some authoritative guidance. But when I arrived, they rejected any idea of treatments, saying there wasn’t enough research to justify their use. Instead, they suggested, I should focus on managing my anxiety.
This was news to me. Beyond the stress of my condition, I didn’t feel unusually anxious. “Are you saying the problem’s in my head?” I asked.
“Not at all,” the doctor replied. “But anxiety management can really help a condition like this.” He suggested I join another waiting list for a few sessions of cognitive behavioural therapy (CBT).
It was a huge disappointment, yet as I left the clinic, I felt relieved, even elated. At last I’d been heard. At last, the NHS acknowledged my existence.
Victoria, 13, felt the same. “She came out with a great big grin on her face,” her mum, Sarah, recalled. “And she just said, ‘They believe me. They know I’m in pain and they know it’s real.’ And then we got home and thought, okay, but they can’t do anything. What’s the point of having this diagnosis when they can’t do anything?”
A few days after my appointment, I had the same sinking feeling.
There was no NHS treatment, nor any prospect of one on the horizon. When I mentioned drugs that had helped other people, including ones being investigated by research trials, the doctors dismissed it as a placebo effect. There were no brain scans or tests of mitochondrial function. All roads, for people with my set of symptoms, led to a course of CBT.
Why weren’t there more treatments for the clinics to offer?
When COVID-19 emerged in early 2020, it was an entirely new virus, yet within 12 months scientists had produced three extremely effective vaccines and discovered several excellent treatments. More than two years after patients first began drawing attention to it, there was nothing even remotely comparable for long COVID.
I found an answer when I spoke to Dr Charles Shepherd, honorary medical adviser to the ME Association. In the late 1970s, he was a fit young doctor in his early thirties working long days in Cirencester Hospital, when he caught chickenpox from a patient. The chickenpox went away, but Dr Shepherd never recovered. Instead, he was left with “activity induced fatigue, brain fog, problems with short term memory, concentration, attention span, processing information”, a condition eventually diagnosed as myalgic encephalomyelitis (ME).
The list of symptoms was all too familiar. Forty years apart, Dr Shepherd and I had been struck down by almost identical diseases, and – what was worse – been met with very similar responses. Dr Shepherd was a medical mystery. So was I.
In the four decades between our collapses, almost no progress had been made on uncovering the nature of post-viral disease.
The reason was not hard to find. “ME was regarded as hysterical nonsense by the medical profession,” said Dr Shepherd, recounting how he’d been ignored and dismissed by his fellow practitioners. Even when grudging acceptance came, it wasn’t followed by funding for research.
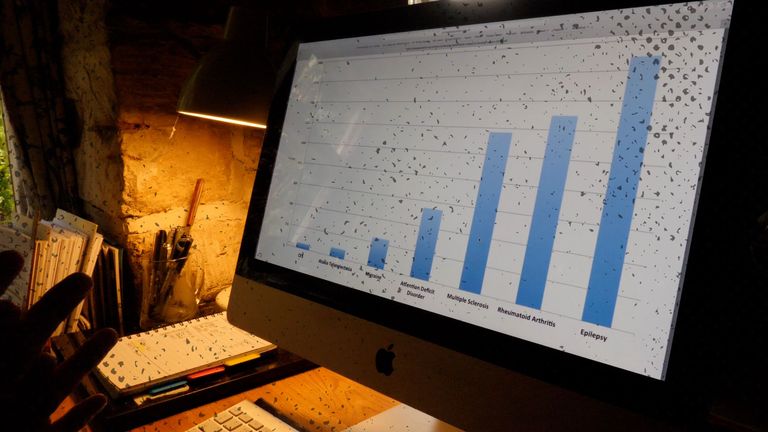
Sky News analysis found that in the 20 years before the pandemic, there were just 2,007 new scientific publications on ME/CFS.
Over the same period, by comparison, there were nearly 45,000 publications investigating the skin condition psoriasis and 114,000 on the topic of Parkinson’s.
Per sufferer, as the chart below shows, ME/CFS receives a fraction of the research of other similar conditions, despite evidence that it reduces quality of life by a greater amount.
I asked Dr Shepherd: if there’d been sufficient funding for ME/CFS, could we have a treatment for my kind of long COVID?
“I think the answer is, yes we could,” he replied. “What we’ve had is a period of tremendous missed opportunity because of lack of interest, lack of funding.”
Funding has been growing.
The National Institutes for Health estimate that ME/CFS research will receive $17m a year in 2022 and 2023, a two-fold increase, although as the chart below shows, that’s still just 4% of the $472m that researchers estimate should be allocated each year, at a minimum, to match the disease’s social burden.
Money has also been going into research for long COVID, including the many symptoms that do not obviously resemble ME.
But after a brief acceleration during the pandemic, research has gone back to its usual crawl, and funding awards often favour psychological pick-me-ups over cutting-edge science. (A study investigating whether weight loss could help long COVID recently received £1 million from the National Institute for Health Research.)
It felt good to understand why there wasn’t more treatment on offer, but my investigation brought me little comfort. Unless a large-scale research drive is launched, the hard reality for most sufferers like me is that there is little chance a scientifically-backed treatment will arrive any time soon. We’ll have to make do with what we have.
The person who eventually pulled me out of my long COVID hole was called Dr Julie Denning.
She was a vocational rehabilitation specialist – a health coach – provided by my insurance company. She worked for a company called Working to Wellbeing.
When I first heard I was getting a health coach, I rolled my eyes. I wanted drugs or treatments, not advice on scheduling. “I am a grown up,” I thought. “I can manage my own time.”
But I couldn’t. I couldn’t stop pushing myself in ways that were hurting my recovery. I couldn’t get out of the cycle of energy boom and bust.
Dr Denning could.
She stood between my bosses and me, giving us both a schedule, one that adapted to my condition rather than the other way around. For the first six months it didn’t change at all, but Dr Denning stopped me losing touch with work and losing hope. She was part human resources officer, part counsellor, part nurse.
Above all, she taught me to accept my situation. Instead of fighting my condition, I began to work with it. I learnt how to identify my brain slowing – a word forgotten, a simple action suddenly grown confusing – and stop before things got worse. It wasn’t easy, but I was learning the fine art of pacing.
With her guidance, I gradually began to improve. I did half days at work, then consecutive half days, then two-thirds of a day. Eventually I was able to take on the project you’re reading now. It was completed over a number of weeks with regular breaks, but it was completed. That felt huge.
In the absence of scientifically verified treatment, this is the kind of support the long COVID clinics might offer, calibrated to each of the condition’s many symptoms. At present, most do not.
The standard of clinics varies hugely across the country and some truly are centres of excellence, yet most offer no help with work, nor assistance beyond a few core symptoms.
“We need a different model,” says Dr Elaine Maxwell. “There are people out there every day helping people with brain fog. None of them are working in the long COVID clinics as far as I can see. It’s the same with other disciplines. We are not making the best use of the knowledge we have.” Most clinics do not have specialists in postural tachycardia or mast cell activation syndromes, for instance, despite their well-established connection to long COVID.
Dr Maxwell, the author of two NIHR studies into long COVID, wants the clinics to echo other specialisms and introduce clinical nurse specialists to take responsibility for patients’ care, providing immediate practical assistance and directing them to the best help available across the NHS. For a group that is often stressed, fatigued and not necessarily thinking straight, that kind of help can be lifesaving.
There are other sources of support for long COVID sufferers, such as groups like Long COVID Support or Long COVID Kids, which has been a lifeline for Victoria and her mum Sarah. “When people come to our group, the first thing they say is they don’t feel alone,” says Jo Moore of Long COVID Support.
But all too often it feels like an uphill battle just to get simple help, or to get recognition from employers, pension funds or government agencies. Despite all the press attention and all the testimonies, it often feels as if people still don’t quite believe long COVID exists.
I am not better now. I may never get better.
But I know that if I am careful and work within my limits, I can work, accomplish tasks and find pleasure with my friends and family. I can live, rather than simply existing.
That may not be everything I wanted, but it is something. Everyone deserves a chance to have something.
Additional reporting by Ben van der Merve